Source: Center for Animal Health and Food Safety
What we’ve learned so far
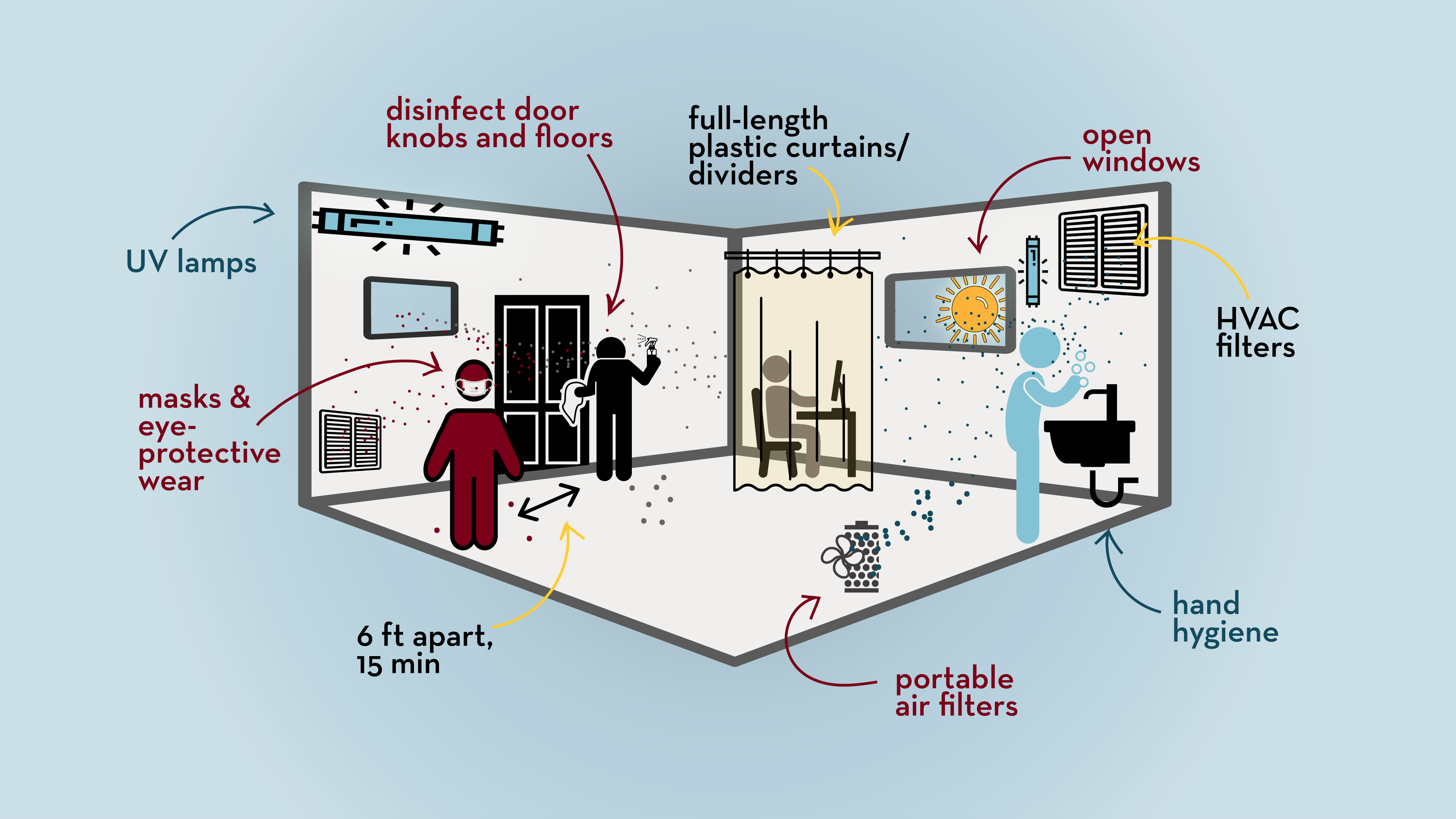
Eight months into the COVID-19 pandemic and the struggle to reduce disease transmission is real. While there is no one size fits all solution, scientists have emphasized the importance of layering multiple protective measures instead of relying on one.
We now know that SARS-CoV-2, the virus that causes COVID-19, transmits directly through close contact and is able to hitchhike with droplets or aerosols and land on nearby objects or enter the respiratory tract of those people in close proximity. Risk-based preventive approaches such as creative use of space, wearing masks, avoiding large gatherings, washing hands, and improving ventilation have been suggested as key to reduce the risk.
As Dr. Anthony Fauci of the Nation Institute of Allergy and Infectious Diseases suggested, “outdoors are preferable” to achieve the goals of better ventilation and physical distancing. However, with winter at our doorsteps, indoors cannot be avoided.
There are many uncertainties—yet based on available knowledge, listed here are eight suggestions to help reduce the spread of COVID-19.
1. Space and time matters
Recommendation: 6 feet for 15 minutes or less
Both thresholds represent a wide range of distances and periods, and yet help define what we call a ‘close contact’ for aerosol transmission. Conversations that last over 15 minutes or if people are simply in the same room with others beyond that length of time, even with masks and distancing, will end up sharing each other's aerosolized breath.
Ideas: Plan shorter trips to the grocery store. Limit time spent in crowded places.
2. Open windows
Recommendation: Sufficient and effective ventilation
Improving indoor ventilation with outside air by opening windows or operating window air conditioners with an outdoor vent are simple measures that could dilute the concentration and reduce the risk of breathing an infectious dose of the virus. Ventilator placement defines the flow pattern, with the objective to increase the airflow and to achieve a directional ‘clean-to-dirty’ airflow where infectious aerosols are captured and exhausted.
Ideas: Open windows when possible.
3. HVAC filters and portable air purifiers
Recommendation: Improve building air filtering status and clean floors
The heating, ventilation, and air-conditioning (HVAC) systems of buildings are designed to control temperature and relative humidity. When HVAC systems have MERV-13 or greater, ULPA, or hospital-grade HEPA filters, which filter particles larger than 0.3 microns, they can reduce airborne contaminants like dust or pollen. While the virus itself is much smaller, the aerosols or droplets containing the virus are in the size range that is possible to filter through these.
Through consultation with building and HVAC designers, ventilation and air purification can be improved. However, only a small percentage of aerosols remain suspended in the air leaving the majority to land on the floor and surfaces, highlighting the importance of cleaning the floors and surfaces.
Portable air purifiers/sanitizers equipped with HEPA filters or UV irradiation can further improve air quality indoors. However, while potentially contributing to the reduction of viral concentration, by themselves portable air cleaners and HVAC filters are not enough to protect people from SARS CoV-2 virus (Additional guidance: ASHRAE).
Ideas: Check your building’s air filtering status. Portable air purifiers may be useful.
4. Room dividers
Recommendation: Additional barriers with full-length plastic curtains
Crowded workplaces, such as meat processing plants, have been using dividers between workstations to add protection. Though lacking studies specific to SARS CoV-2, a study conducted in 2004 suggested that full-length plastic curtains and portable air filtration units were useful in creating a ‘zone-within-zone’ to reduce the risk of aerosol transmission.
Ideas: Because household transmission is a significant source, if you are isolating at home divide your room with plastic curtains.
5. How many people at a time?
Recommendations: 100 – 150 sq ft per person at work
Though debatable, some suggest reducing risk through managing the number of people sharing a room. Recommendations range from 100 to 250 sq ft per person; the Federal Emergency Management Agency (FEMA) suggests 100 – 150 sq ft per person in an office.
Another tricky question is what to do about asymptomatic individuals, because they’re capable of transmitting the disease just as much as to a person who is coughing or sneezing would. This emphasizes the importance of wearing protective gear regardless of symptoms. To help tracking down potential exposure to asymptomatic individuals, logging time spent in each room at work may be useful.
Ideas: Imagine approximately a standard parking space (i.e. 180 sq ft) per person.
6. Masks, eye protection, disinfection, and hand hygiene
Recommendation: wear a face masks in public indoor areas
As suggested by multiple studies, wearing a mask reduces the risk of transmission. The effectiveness of face masks varies by the fabric and fit. Medical-grade masks such as N-95/KN95/FFP1/FFP2/FFP3 or similar respirators filter better than fabric or surgical masks and are fitted to the face. However, it is important to reserve these critical supplies for the medical first responders. Our choice of the type of mask varies by availability, price point, fit to the user, and the risk of exposure.
The virus is known to directly transmit from person-to-person through sneezing, coughing, and talking as well as through fomites contaminated with virus. Therefore, practicing hand hygiene, sanitizing, and avoiding touching the mouth, nose, or eyes are emphasized. Good hand hygiene would also act protectively against the potential fecal-oral transmission route of SARS CoV-2. The EPA suggests safety guidelines for routine cleaning of the shared surfaces. While air disinfection was advised, if done too frequently it may cause irritation in eyes and nose.
Ideas: Disinfect shared doorknobs, tables, and elevator buttons. Wear a mask covering both nose and mouth, and a face shield if you are at risk (e.g. work at a grocery store or wait tables at a restaurant).
7. Lessons from other disciplines
Recommenation: Look beyond human health for other scientific studies and recommendations.
Aerosol transmission is not COVID-unique. The scientific confirmation of aerosol transmission of a virus and the factors supporting the transmission is challenging, because the virus’s ability to remain alive and infective changes due to the ambient temperature, relative humidity, UV-radiation/sun light and the variation of research method used.
While scientific studies are on the way to add more knowledge on COVID-19, studies from other disciplines such as veterinary practices indicate that when aerosol transmission of viruses are considered, transmission is not limited to a shared room.
Aerosol transmission of respiratory viral diseases in pigs was observed to transmit between rooms that are over 1 meter apart but connected with air ducts, connecting airflow. While different viruses would behave differently, it is important to know the engineering of the ventilation systems and connectivity between rooms to plan improved ventilation and air sanitation.
8. Beware of the risk compensation behavior
Recommendation: Self-isolate and test if you suspect exposure
The behavior of empathy should be applauded. A few things we could do are following the CDC guidelines for quarantine, testing, and self-isolating when we suspect exposure to an infected person; answering the call from the local health department; opting for virtual meetings; and choosing outdoors when possible.
The risk of person-to-person transmission of infectious diseases is complex. While creating a ‘zero risk’ environment is unlikely, practicing redundancy with more than one preventive measure in place is the key to reduce the risk.
